Jeff Naticchia wasn’t feeling well when he set off to work one Friday in late July 2017. The sales supervisor at Comcast was planning to work a half-day before a long-planned family weekend in Upstate New York. Instead, he called his wife, Crissy, from work and said to meet him at the emergency room. Something was wrong.
When Crissy arrived, she was shocked at what she saw: Her husband’s skin was yellowed, he seemed agitated and he couldn’t urinate.
Jeff was turning 51 and had been dieting and exercising to stay in shape, taking long walks in the state park that backed up to their home in Bucks County, Pa. He had always been healthy, although earlier that month, he started getting fevers and night sweats and had gone to a local urgent care clinic. He was given a urine test, diagnosed with a kidney infection and prescribed antibiotics. Briefly, he seemed to improve.
But now, doctors in the ER examined Jeff, ordered tests and, with no immediate answers, admitted him to the hospital.
The next day, Jeff was weaker, sweating, unable to sleep. His breathing was labored. The whites of his eyes had yellowed, and his bilirubin was climbing, a sign that red blood cells were breaking down at an unusual rate or of liver trouble. The doctors moved Jeff to the intensive care unit, and placed him in a medically induced coma and on a ventilator. On Sunday, he was transferred to a hospital specializing in liver care.
Jeff’s symptoms resembled malaria. Could he have caught something in Costa Rica three months earlier? No, that timing didn’t make sense. Jeff was put on kidney dialysis. His team periodically woke him, and he would squeeze his wife’s hand.
Finally, on Tuesday, some potentially good news. An infectious-disease doctor at the hospital told Crissy, “We think we have a diagnosis.”
Jeff probably had babesiosis, a tick-borne infection that attacks red blood cells and appears to be growing in prevalence. Were there a lot of ticks or deer in her yard? Yes, she said, and later recalled that Jeff had pulled a tick off himself that summer, no bigger than a poppy seed. The doctor ordered an antibiotic and blood transfusion. Jeff’s condition was serious, he told her, but he was cautiously optimistic.
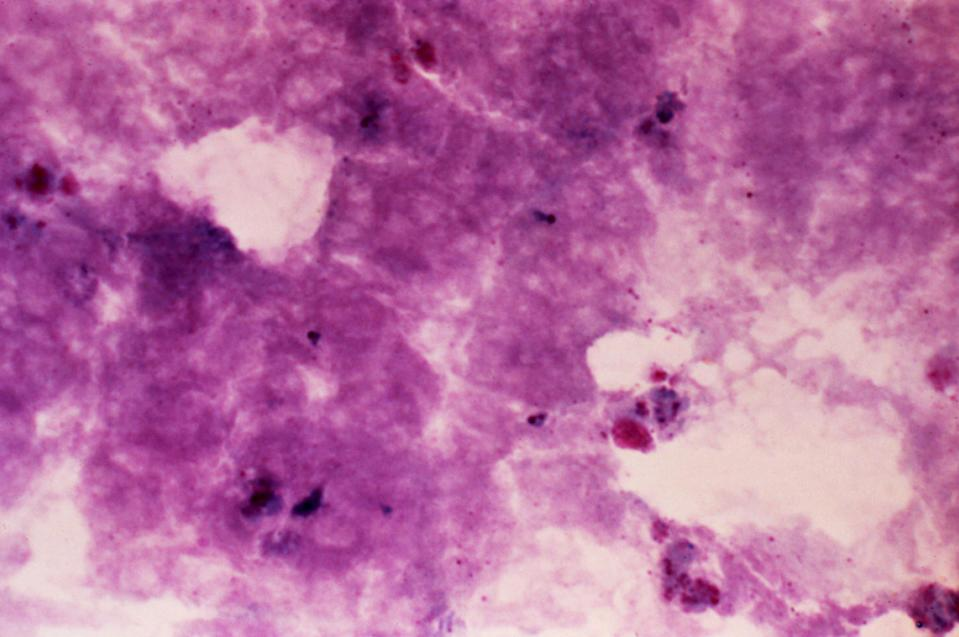
Babesiosis is most often caused by the tiny parasites Babesia microti and transmitted to humans in warmer months by deer ticks - the same ones that spread Lyme disease. It is rarely passed through blood transfusion.
Most U.S. cases occur in the Northeast and Upper Midwest, but babesiosis does appear elsewhere, according to the Centers for Disease Control and Prevention. Peter Krause, a senior research scientist at Yale School of Public Health and Yale School of Medicine, said that babesiosis is “increasing in frequency and geographic range.”
A recently published 12-year study of babesiosis among U.S. Medicare beneficiaries reported “substantially increasing babesiosis diagnosis trends” particularly in endemic states and “expansion of babesiosis infections in other states.”
In 2011, when the CDC began collecting data on babesiosis, 1,126 cases were reported. Today, over 2,000 cases of babesiosis are reported in the United States each year, although Krause said he believes the actual number is many times higher. He explained: Lyme is underreported by more than tenfold, both diseases are spread by the same tick, and babesiosis is harder to diagnose. While 30,000 cases of Lyme are reported each year, the CDC estimates the actual number to be closer to 476,000.
“Most diseases are underreported because the system relies on physicians sending in reports of cases and physicians are busy,” Krause said. Babesiosis may also go unreported due to asymptomatic and misdiagnosed infections, and reporting not being mandated in all states.
Most people infected with babesiosis are asymptomatic or have mild to moderate flu-like symptoms such as fatigue, chills, sweats, headache, body aches, nausea and loss of appetite, which can appear days or even months later. (There is no telltale rash as with Lyme disease.)
If diagnosed quickly, the disease can be easily treated with a combination of atovaquone and azithromycin for seven to 10 days. If a person’s immune system is impaired, babesiosis can be deadly and the medication will be given longer. Among those most at risk are the elderly; individuals with cancer, AIDS or other serious immunocompromised conditions; people being treated with chemotherapy, high-dose steroids or rituximab, an antibody therapy often used against cancer or autoimmune diseases; or those without a spleen. Jeff’s spleen was removed in childhood after a bike accident.
If Jeff had been diagnosed early, when he first complained of night fevers, it might have been different for him. But at 4 a.m. on Thursday morning, the hospital called Crissy to tell her his blood pressure was dropping precipitously and she needed to come right away. She left immediately, without waking their children. Jeff died a few hours later.
Krause said “the rate of death among babesiosis patients who are immunocompromised is as high as 20 percent.”
Where babesiosis is not endemic, urgent care and ER providers may not immediately think of the disease when someone comes in, since the symptoms can point to many things and none of them are specific to babesiosis. It requires a specific type of blood test to identify the parasite in red blood cells.
“It has to step up to the level of an infectious-disease specialist being brought in before it might get diagnosed, whereas in an area where it’s more prevalent, some of the front-line people, the emergency room doctors or urgent care doctors, might be a little more attuned to it,” said infectious-disease specialist Sorana Segal-Maurer, director of the Dr. James J. Rahal Jr. Division of Infectious Diseases at NewYork-Presbyterian Queens hospital.
Gary Wormser, chief of infectious diseases at New York Medical College and director and founder of the Lyme Disease Diagnostic Center, said deer ticks may transmit several diseases, including Lyme, babesiosis and anaplasmosis, which has symptoms and risk factors similar to babesiosis but is generally treated with a different medicine, doxycycline. With Lyme disease and babesiosis, he said, “the ticks have to be on you for a fairly long time before they transmit those particular infections.”
Chances of avoiding infection are likely if the tick is removed within 24 to 36 hours. After possible exposure to deer ticks, Wormser advised showering within two hours, running clothes in a hot dryer for at least 10 minutes and doing a total body check for ticks on the skin within 24 hours.
If you find a tick, the CDC recommends removing it with fine-tipped tweezers, grasping the tick close to the skin and pulling upward with steady pressure.
Since Jeff’s death, Crissy and her kids have worked to raise awareness of babesiosis, hoping to prevent other families from experiencing the heartbreak of losing a loved one.
Crissy said it is important to get out in nature - especially now with the pandemic having forced so many restrictions. But for those who live in areas where ticks are common, she said it is important to check your body for ticks when you come home.
Source: The Washington Post